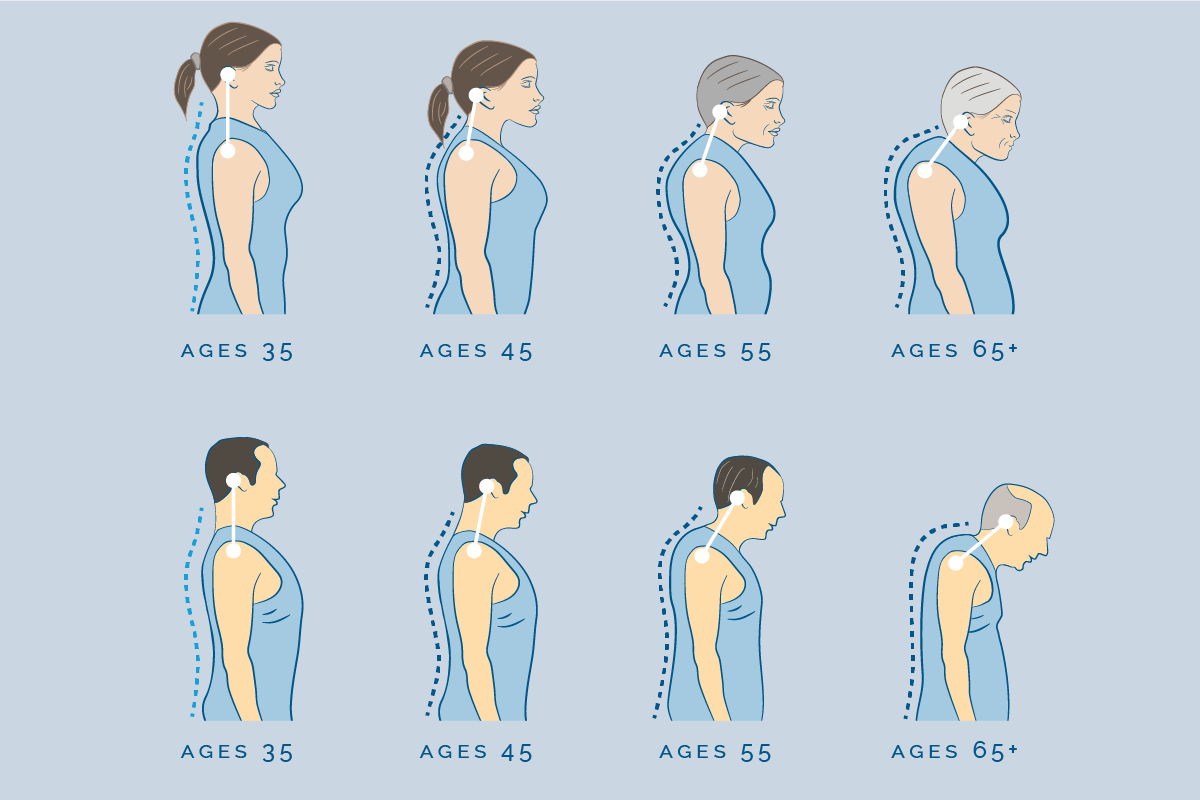
As the decades accrue, the concern over bone health shifts from an abstract notion to a concrete, daily reality. The silent erosion of bone mineral density, a process called osteopenia, progresses toward osteoporosis, dramatically increasing the risk of a fracture from what would otherwise be a minor stumble—a fragility fracture. These breaks, particularly of the hip or spine, are often devastating, frequently marking a sharp and irreversible decline in independence and overall quality of life. Preventing them, therefore, is not merely about consuming a specific supplement but requires a holistic and persistent strategy that engages every aspect of daily living, from the molecular dynamics within the bone matrix to the spatial arrangement of furniture in one’s home. The conventional wisdom often simplifies the solution down to calcium and vitamin D, yet this perspective misses the mark by overlooking the non-linear, interconnected factors of muscle strength, balance, environmental hazards, and the often-overlooked influence of various medications. Adopting an integrated, multi-faceted approach is the only reliable path to fortifying the skeleton against the inevitable challenges of aging.
The silent erosion of bone mineral density, a process called osteopenia, progresses toward osteoporosis, dramatically increasing the risk of a fracture from what would otherwise be a minor stumble—a fragility fracture.
The conventional wisdom often simplifies the solution down to calcium and vitamin D, yet this perspective misses the mark by overlooking the non-linear, interconnected factors of muscle strength, balance, environmental hazards, and the often-overlooked influence of various medications.
The bone is a dynamic, living tissue constantly undergoing a process of remodeling, where old bone is resorbed and new bone is formed. The conventional wisdom often simplifies the solution down to calcium and vitamin D, yet this perspective misses the mark by overlooking the non-linear, interconnected factors of muscle strength, balance, environmental hazards, and the often-overlooked influence of various medications. In youth, formation outpaces resorption, building up the skeletal bank account; however, as one ages, this balance tips, and withdrawal often exceeds deposits. The twin pillars of calcium and Vitamin D are undeniably crucial because the body cannot absorb calcium, the fundamental building block of bone, without the active form of Vitamin D. Yet, simply increasing intake may not be enough. The effectiveness of any calcium and Vitamin D regimen is highly dependent on an individual’s existing nutritional status, their capacity for absorption—which often declines with age—and their exposure to sunlight. Furthermore, there is a complex, almost counterintuitive dose-response curve, where excessive supplementation without addressing deficiencies in other cofactors can offer diminishing returns or even pose other health risks, especially for those with existing cardiac concerns or a history of kidney stones.
The effectiveness of any calcium and Vitamin D regimen is highly dependent on an individual’s existing nutritional status, their capacity for absorption—which often declines with age—and their exposure to sunlight.
The bone is a dynamic, living tissue constantly undergoing a process of remodeling, where old bone is resorbed and new bone is formed and new bone is formed.
While the structure of the bone itself is paramount, the vast majority of fractures do not happen because the bone spontaneously gives way; they occur because of a fall. The effectiveness of any calcium and Vitamin D regimen is highly dependent on an individual’s existing nutritional status, their capacity for absorption—which often declines with age—and their exposure to sunlight. Therefore, shifting the focus from simply increasing bone density to reducing the frequency of falls represents a far more immediate and impactful strategy for prevention. Falls are most often triggered not by a single misstep but by a gradual decline in neuromuscular function, encompassing everything from diminished reaction time to profound loss of proprioception—the body’s internal sense of where it is in space. Muscle strength, particularly in the lower extremities, is not just about power; it is the ultimate stabilizer, providing the fast, reflexive corrections necessary to catch oneself mid-stumble.
Falls are most often triggered not by a single misstep but by a gradual decline in neuromuscular function, encompassing everything from diminished reaction time to profound loss of proprioception—the body’s internal sense of where it is in space.
Therefore, shifting the focus from simply increasing bone density to reducing the frequency of falls represents a far more immediate and impactful strategy for prevention.
To mitigate this decline in stability, a comprehensive exercise program must move beyond general walking or light cardio and deliberately target the muscles and neural pathways responsible for maintaining upright posture. Falls are most often triggered not by a single misstep but by a gradual decline in neuromuscular function, encompassing everything from diminished reaction time to profound loss of proprioception—the body’s internal sense of where it is in space. Programs like Tai Chi, which emphasizes slow, controlled movements and weight shifting, have repeatedly demonstrated superior results in improving static and dynamic balance compared to standard stretching routines. Additionally, resistance training, using weights, bands, or even bodyweight, is essential for combating sarcopenia, the age-related loss of muscle mass and strength. This targeted strengthening is crucial, as stronger muscles act as natural shock absorbers, better protecting bones upon impact and, more importantly, providing the necessary foundation for swift recovery from a momentary loss of balance.
Programs like Tai Chi, which emphasizes slow, controlled movements and weight shifting, have repeatedly demonstrated superior results in improving static and dynamic balance compared to standard stretching routines.
To mitigate this decline in stability, a comprehensive exercise program must move beyond general walking or light cardio and deliberately target the muscles and neural pathways responsible for maintaining upright posture.
An often-underestimated source of fall risk resides not in the body, but in the environment—specifically, the home. Programs like Tai Chi, which emphasizes slow, controlled movements and weight shifting, have repeatedly demonstrated superior results in improving static and dynamic balance compared to standard stretching routines. While a fall outside is often unpredictable, up to half of all falls in older adults occur within their own residence, making hazard mitigation a high-yield preventive measure. This involves a systematic audit of the living space to identify trip and slip hazards that are easily ignored out of habit. Loose rugs, poor lighting in stairwells, power cords snaking across pathways, and the absence of grab bars in wet areas like bathrooms all contribute to an elevated baseline risk. Simple, cost-effective adjustments, such as securing rugs with double-sided tape, installing motion-sensor lighting, and moving frequently used items to easily accessible shelves, can fundamentally alter the safety profile of a person’s daily routine, effectively neutralizing numerous opportunities for a catastrophic fall.
This involves a systematic audit of the living space to identify trip and slip hazards that are easily ignored out of habit.
An often-underestimated source of fall risk resides not in the body, but in the environment—specifically, the home.
The pharmacological landscape of aging introduces yet another layer of complexity. This involves a systematic audit of the living space to identify trip and slip hazards that are easily ignored out of habit. Many common medications prescribed for unrelated conditions inadvertently increase fracture risk, primarily by affecting balance, cognition, or blood pressure. Classes of drugs such as certain antidepressants, sedatives, benzodiazepines, and even some antihypertensives can cause dizziness, orthostatic hypotension (a drop in blood pressure upon standing), or general drowsiness, all of which directly impair the body’s ability to maintain stability and react quickly to a trip. A crucial, yet frequently missed, preventative step is a comprehensive medication review conducted by a pharmacist or physician specializing in geriatrics. This review should aim to de-prescribe unnecessary medications or switch to alternatives that have a lower central nervous system impact, thereby reducing the pharmacological burden on balance.
Classes of drugs such as certain antidepressants, sedatives, benzodiazepines, and even some antihypertensives can cause dizziness, orthostatic hypotension (a drop in blood pressure upon standing), or general drowsiness.
The pharmacological landscape of aging introduces yet another layer of complexity.
Beyond the physical and environmental, the neurological and sensory components of balance cannot be ignored. Classes of drugs such as certain antidepressants, sedatives, benzodiazepines, and even some antihypertensives can cause dizziness, orthostatic hypotension (a drop in blood pressure upon standing), or general drowsiness. The ability to navigate space relies heavily on three primary senses: vision, proprioception, and the vestibular system in the inner ear. Age-related decline in visual acuity, particularly depth perception and contrast sensitivity, means that small changes in floor level or poorly lit steps become enormous obstacles. Similarly, impairments in the vestibular system, which processes motion and head position, can lead to chronic instability. Regular vision checks, the use of appropriate corrective lenses—with an important note to be cautious with progressive lenses during stair use—and, where indicated, vestibular rehabilitation exercises are necessary interventions that act as high-levers in fracture prevention by refining the body’s essential navigational equipment.
The ability to navigate space relies heavily on three primary senses: vision, proprioception, and the vestibular system in the inner ear.
The neurological and sensory components of balance cannot be ignored.
The concept of weight-bearing exercise offers a direct, mechanical solution to the problem of diminishing bone density. The ability to navigate space relies heavily on three primary senses: vision, proprioception, and the vestibular system in the inner ear. Bone, like muscle, responds to stress; it adapts to the forces placed upon it by becoming stronger and denser—a process governed by Wolff’s Law. Non-impact activities like swimming or cycling, while excellent for cardiovascular health, do not provide the necessary mechanical load to stimulate significant bone growth or maintenance. Activities that force the body to work against gravity, such as brisk walking, jogging, stair climbing, and specific resistance exercises like squats and lunges, send potent signals to the bone cells to fortify the structure. The key is consistency and progression, ensuring the load is gradually increased over time to continue challenging the skeleton without exceeding its capacity and causing injury.
Bone, like muscle, responds to stress; it adapts to the forces placed upon it by becoming stronger and denser—a process governed by Wolff’s Law.
The concept of weight-bearing exercise offers a direct, mechanical solution to the problem of diminishing bone density.
Finally, the most critical step in this entire preventative framework is early and accurate risk stratification. Bone, like muscle, responds to stress; it adapts to the forces placed upon it by becoming stronger and denser—a process governed by Wolff’s Law. The majority of individuals who suffer a fragility fracture have never been screened for osteoporosis. Tools like the FRAX calculator, which estimates the 10-year probability of a major osteoporotic fracture based on clinical risk factors, and the Dual-Energy X-ray Absorptiometry (DEXA) scan are essential for identifying those most at risk before the first fracture occurs. A diagnosis of osteoporosis is not a final verdict, but a prompt for aggressive, customized intervention, often involving prescription bone-building or anti-resorptive medications, in addition to all the lifestyle and environmental changes mentioned previously. Fracture prevention is a proactive task, demanding continuous monitoring and a personalized strategy that evolves with age.