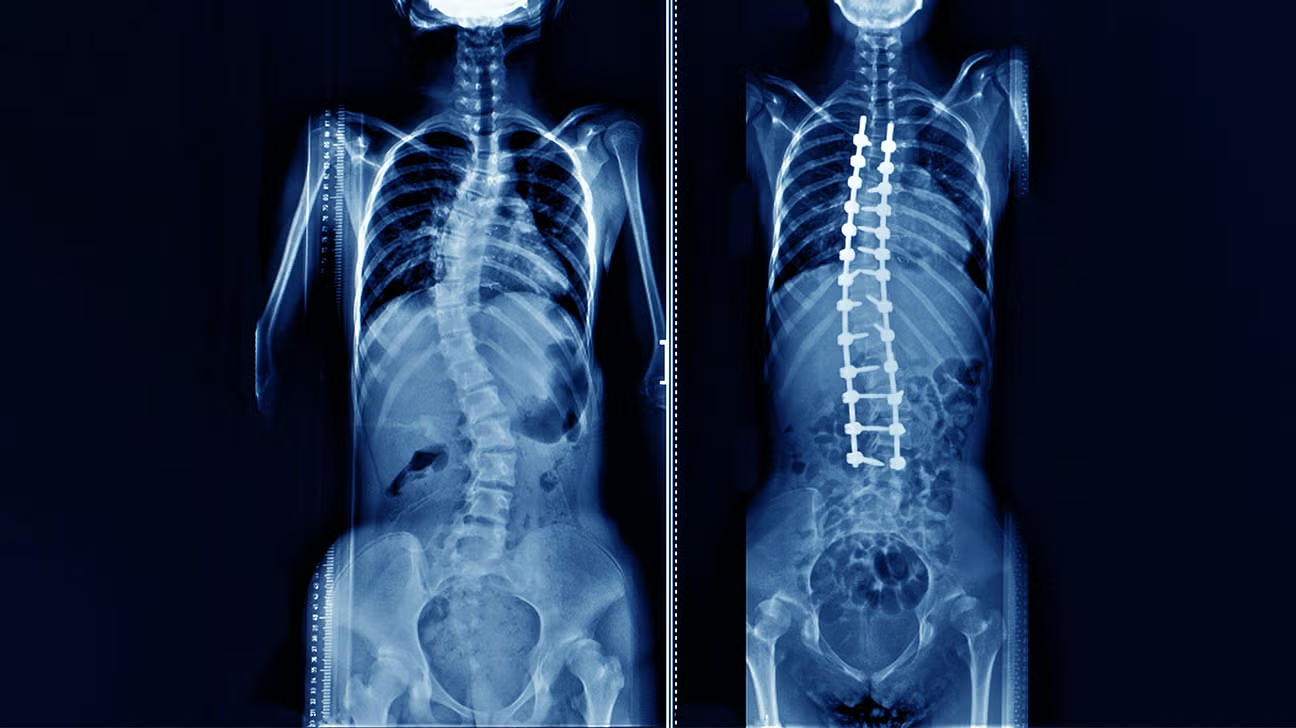
The prospect of spinal fusion surgery represents a profound pivot point for individuals contending with chronic, debilitating axial or radicular pain originating from vertebral instability or deformity. This procedure, fundamentally a biological welding process, is the deliberate act of eliminating motion between two or more vertebrae, compelling them to grow together into a single, rigid bone segment. It is far from a trivial decision, often reserved as a last resort when a comprehensive course of non-operative therapies—including targeted physical rehabilitation, pharmaceutical management, and interventional pain procedures—has failed to provide satisfactory and enduring relief. The core objective is to stabilize a painful segment, either due to a congenital defect, traumatic injury, severe degenerative change, or a progressive spinal curvature like scoliosis or kyphosis. Yet, the choice to pursue fusion necessitates a rigorous understanding of its biomechanical consequences, the nuanced technical variations employed by surgeons, and a sober assessment of the realistic trajectory of recovery, which is measured in months, not weeks.
This procedure, fundamentally a biological welding process, is the deliberate act of eliminating motion between two or more vertebrae
The decision matrix for recommending spinal fusion is inherently intricate, moving well beyond the simple presence of anatomical pathology on imaging scans. “This procedure, fundamentally a biological welding process, is the deliberate act of eliminating motion between two or more vertebrae” precisely defines the mechanism, but the why is more complex. A successful outcome hinges not merely on achieving solid bony union, known as arthrodesis, but on accurately identifying the specific spinal segment or segments generating the patient’s pain. Indications for fusion are diverse and include severe spondylolisthesis—the forward slippage of one vertebra over another—unstable vertebral fractures, severe discogenic pain, and conditions causing mechanical instability following extensive decompression procedures. However, the patient’s overall physiological status, bone density, and capacity for healing are equally critical determinants. A meticulous surgeon will spend significant time confirming that the targeted segment is indeed the primary source of symptoms, often through diagnostic nerve blocks or selective discography, before committing to a permanent alteration of the spinal architecture.
A meticulous surgeon will spend significant time confirming that the targeted segment is indeed the primary source of symptoms
Spinal fusion is not a monolithic procedure; rather, it is a classification encompassing numerous surgical techniques differentiated primarily by the access route and the method of placing the bone graft material. “A meticulous surgeon will spend significant time confirming that the targeted segment is indeed the primary source of symptoms” leads directly into the necessity of choosing the correct approach. Surgeons may choose an anterior approach (through the abdomen or front of the neck), a posterior approach (from the back), or a lateral approach (from the side, avoiding major abdominal and posterior musculature). The choice of technique, such as Posterior Lumbar Interbody Fusion (PLIF), Transforaminal Lumbar Interbody Fusion (TLIF), or Anterior Lumbar Interbody Fusion (ALIF), is dictated by the specific pathology, the requirement for direct disc removal or nerve root decompression, and the degree of lordosis—the natural inward curve of the lower back—that needs to be restored. Each access corridor carries its own distinct set of associated risks, from potential vascular or visceral injury in the anterior approaches to greater muscle dissection and blood loss with traditional posterior incisions.
The choice of technique, such as Posterior Lumbar Interbody Fusion (PLIF), Transforaminal Lumbar Interbody Fusion (TLIF), or Anterior Lumbar Interbody Fusion (ALIF), is dictated by the specific pathology
A non-negotiable component of any spinal fusion is the bone graft material, which serves as the biological scaffolding for the new bone growth that achieves the final, solid union. “The choice of technique, such as Posterior Lumbar Interbody Fusion (PLIF), Transforaminal Lumbar Interbody Fusion (TLIF), or Anterior Lumbar Interbody Fusion (ALIF), is dictated by the specific pathology” transitions logically into the material science of the procedure. Traditionally, autograft, bone harvested from the patient’s own body—most commonly the iliac crest—has been considered the gold standard due to its intrinsic osteoinductive (growth-stimulating) and osteoconductive (scaffolding) properties. However, this method introduces a second surgical site with its own risk of chronic pain. Modern spine surgery frequently utilizes allograft (donor bone), or synthetic alternatives combined with various biological enhancers like bone morphogenetic proteins (BMPs) to stimulate bone growth without the morbidity of a separate harvest procedure. The efficacy of the fusion, often referred to as the fusion rate, is heavily dependent on the quantity and quality of this graft material.
The efficacy of the fusion, often referred to as the fusion rate, is heavily dependent on the quantity and quality of this graft material.
Instrumentation, typically involving titanium or PEEK (polyetheretherketone) rods, screws, plates, and interbody cages, plays a crucial role not in achieving the final fusion, but in providing immediate, rigid segmental stability until the biological process is complete. “The efficacy of the fusion, often referred to as the fusion rate, is heavily dependent on the quantity and quality of this graft material” highlights the biological process, but metal implants manage the mechanical stress. This hardware functions as an internal splint, reducing movement to less than one millimeter, which is the necessary condition for the bone cells to bridge the gap between the vertebrae. Without such rigid stabilization, the constant micromotion would prevent bone formation, resulting in a failed fusion, or “pseudarthrosis.” Modern surgical advancements have increasingly focused on minimally invasive techniques, utilizing smaller incisions, specialized retractors, and intra-operative navigation systems, which aim to reduce the soft tissue and muscle trauma associated with traditional open surgery, potentially leading to faster initial recovery and less post-operative pain.
This hardware functions as an internal splint, reducing movement to less than one millimeter, which is the necessary condition for the bone cells to bridge the gap
The immediate post-operative period is characterized by acute pain management and initial mobilization, a phase often requiring a hospital stay of several days. “This hardware functions as an internal splint, reducing movement to less than one millimeter, which is the necessary condition for the bone cells to bridge the gap” emphasizes the mechanical role of the hardware, but the patient experience immediately after is dominated by tissue injury. Patients are typically encouraged to walk within a day of surgery, though with strict limitations on bending, lifting, and twisting movements to protect the healing process. The first few weeks are a delicate balance of managing incisional and deep muscle pain, which can be significant, while avoiding activity that could compromise the graft. Full biological fusion, the actual joining of the bones, is a slow process that often takes between three to six months to achieve a radiographically solid union, with total remodeling continuing for a year or more. This extended, non-linear recovery timeline often catches patients by surprise, making realistic expectation setting paramount.
The first few weeks are a delicate balance of managing incisional and deep muscle pain, which can be significant
A frank discussion of the potential risks and long-term implications is mandatory before any patient consents to the operation. “The first few weeks are a delicate balance of managing incisional and deep muscle pain, which can be significant” addresses short-term discomfort, but the long-term changes are more profound. Common risks include wound infection, nerve root injury, excessive blood loss, and the ever-present risk of pseudarthrosis, which necessitates revision surgery. A unique and significant long-term consequence of fusion, particularly in the lumbar spine, is the potential development of Adjacent Segment Disease (ASD). By rigidly fixing one segment, the stress and mechanical load are necessarily transferred to the discs and joints immediately above and below the fused segment. Over the span of years, this increased load can accelerate degenerative changes in these adjacent levels, eventually leading to new instability, pain, and potentially the need for further surgical intervention to extend the original fusion.
A unique and significant long-term consequence of fusion, particularly in the lumbar spine, is the potential development of Adjacent Segment Disease (ASD).
The long-term success of spinal fusion is less about the surgical technique itself and more about the patient’s adherence to a structured, prolonged post-operative rehabilitation protocol. “A unique and significant long-term consequence of fusion, particularly in the lumbar spine, is the potential development of Adjacent Segment Disease (ASD)” outlines a potential failure mode, but successful adaptation is key. Physical therapy, which typically begins a few weeks to months after the procedure, is not merely about regaining strength but involves a fundamental re-education of the body to move effectively and safely with a newly rigid segment. The focus shifts to strengthening core musculature—the deep stabilizers of the trunk—and improving the flexibility of adjacent, unfused segments, such as the hips and thoracic spine, to compensate for the lost motion. A failure to commit to this functional rehabilitation can lead to chronic muscle stiffness, gait abnormalities, and a poorer final functional outcome, even in the presence of a technically solid fusion.
Physical therapy, which typically begins a few weeks to months after the procedure, is not merely about regaining strength but involves a fundamental re-education of the body
The ultimate measure of a successful fusion is not the radiographic image of solid bone, but the patient’s self-reported functional improvement and reduction in chronic pain that resisted all previous treatments. “Physical therapy, which typically begins a few weeks to months after the procedure, is not merely about regaining strength but involves a fundamental re-education of the body” places the emphasis on functional recovery. While the procedure can be genuinely life-altering, offering relief from relentless pain and restoring the ability to participate in many aspects of daily life, it does so by imposing a permanent biomechanical trade-off. Patients must internalize that while the pain may resolve, the fused segment will never move again, and this new mechanical reality dictates a lifelong vigilance regarding body mechanics, weight management, and consistent maintenance of core stability. The decision to proceed is, therefore, a deeply personal equation balancing the severity of current suffering against the enduring, structural modification of the spine.
Patients must internalize that while the pain may resolve, the fused segment will never move again
The landscape of spinal treatment is continuously evolving, with non-fusion alternatives and motion-preserving technologies challenging the dominance of traditional fusion, particularly for single-level degenerative disease. “Patients must internalize that while the pain may resolve, the fused segment will never move again” serves as a powerful final caution about the procedure’s permanence. For instance, total disc replacement (arthroplasty) in the cervical and selected lumbar regions offers the possibility of pain relief while maintaining segment motion, though its long-term durability and efficacy are still subjects of ongoing refinement and debate. Nevertheless, for complex deformities, severe instability, and multi-level disease, spinal fusion remains the established gold standard. The informed patient understands that this surgery is the beginning of a long journey of adaptation, where surgical success is merely the prerequisite for a successful recovery driven by personal commitment and diligent rehabilitation.