Thinking about joint replacement surgery brings a mixture of hope, anxiety, and endless questions. Many people imagine immediate relief, but the reality unfolds more slowly, shaped by many stages. It is not just the procedure itself but the preparation, the emotional toll, and the months of rebuilding afterward. Every person’s journey through joint replacement follows a unique rhythm based on age, health status, and commitment to recovery. Understanding the real pathway helps create better expectations, reduces surprises, and supports stronger outcomes.
Modern joint replacement surgeries aim to restore function, reduce chronic pain, and improve life quality. However, achieving these goals requires patience, teamwork, and careful personal effort long after the hospital stay ends.
Thinking about joint replacement surgery brings a mixture of hope anxiety and endless questions
Preparing for surgery often begins months before the actual date gets scheduled. Consultations, diagnostic tests, and physical assessments shape the first steps of the journey. Surgeons evaluate bone structure, ligament integrity, and surrounding tissue health through imaging and hands-on exams. Patients also undergo general health screenings to minimize surgical risks linked to heart, lung, or metabolic conditions. Weight management, smoking cessation, and diabetic control programs sometimes become part of pre-surgical optimization. Emotional readiness discussions, while less visible, are equally critical for post-surgery satisfaction. A prepared mind adapts faster to pain, temporary setbacks, and the slow pace of rehabilitation ahead.
Modern joint replacement surgeries aim to restore function reduce chronic pain and improve life quality
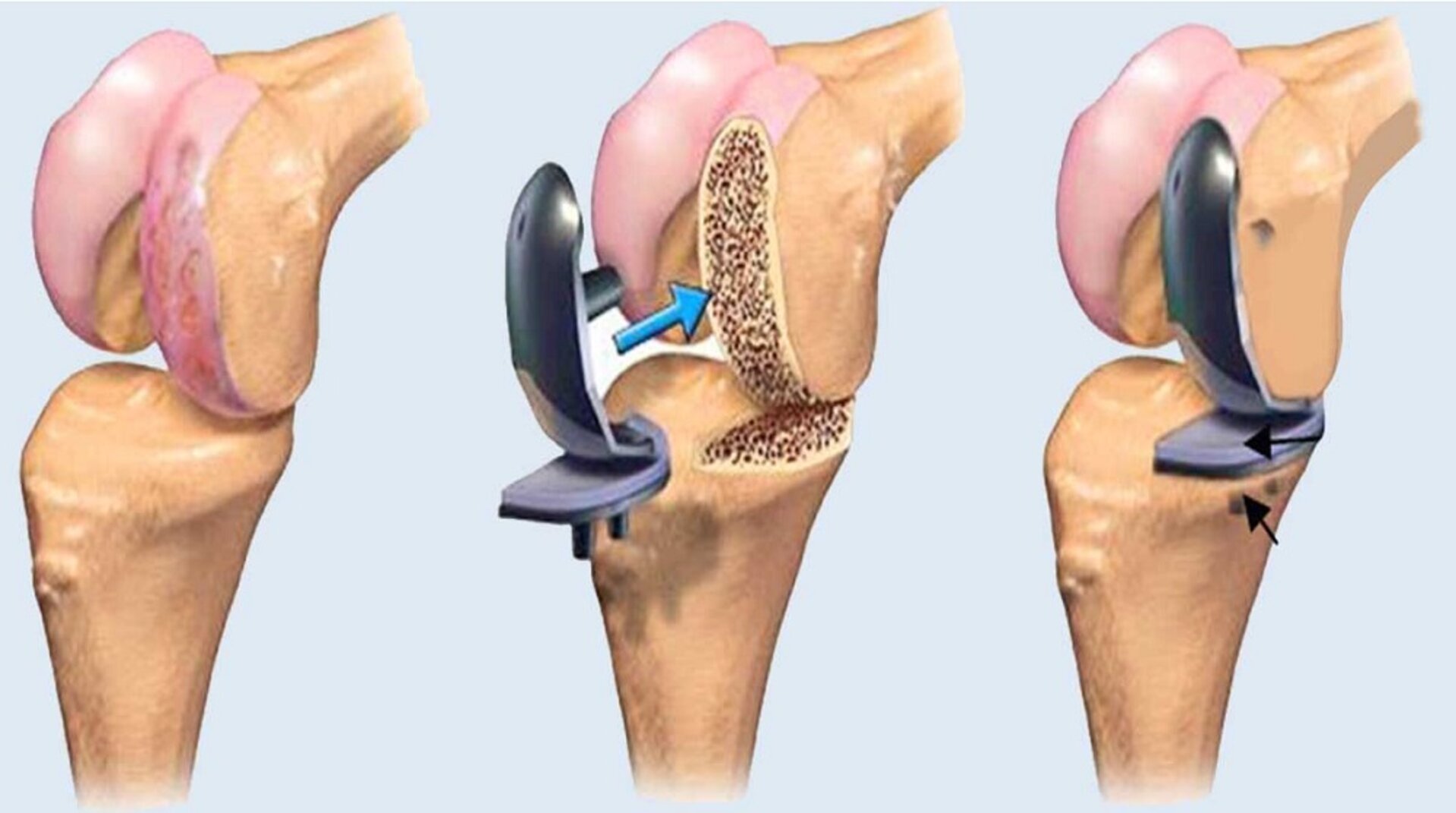
Technological advances have made modern joint replacements safer, more durable, and better tailored to individual anatomy. Customized implants, minimally invasive techniques, and robotic-assisted procedures now enhance precision and reduce tissue trauma. However, no surgery eliminates pain or stiffness immediately after operation. Early days often involve swelling, discomfort, and limited movement capacity. The body’s healing response needs weeks before strength and flexibility begin to return. While long-term results are excellent for most patients, reaching them demands disciplined commitment during recovery phases. Successful outcomes are built through a blend of surgical skill and consistent patient effort afterward.
Preparing for surgery often begins months before the actual date gets scheduled
Long before walking into the operating room, patients navigate a maze of pre-surgical steps. Initial visits focus on identifying eligibility and discussing realistic expectations rather than guaranteeing perfect outcomes. Physicians often recommend strengthening exercises months ahead to condition muscles supporting the affected joint. Learning crutch use, walker navigation, or home safety modifications also happens before surgery day. Psychological preparation includes confronting fears of anesthesia, immobilization, and dependence during early recovery. Anticipating temporary limitations helps minimize post-surgery frustration and improves coping skills when challenges arise. Thorough preparation builds mental resilience alongside physical readiness, critical for successful healing.
Technological advances have made modern joint replacements safer more durable and better tailored to individual anatomy
Despite revolutionary advances, every surgery still carries inherent risks such as infection, blood clots, or nerve injury. Understanding possible complications empowers patients to recognize early warning signs and seek timely interventions. Surgeons today use sophisticated navigation systems to improve implant alignment and longevity. Biocompatible materials reduce allergic reactions and wear, extending the lifespan of artificial joints. Nonetheless, biological tissues require adjustment periods to integrate comfortably with new mechanical components. Some patients experience temporary differences in limb length perception or altered gait patterns during early months. Adapting to these changes forms part of the healing landscape.
Initial visits focus on identifying eligibility and discussing realistic expectations rather than guaranteeing perfect outcomes
Conversations before surgery often feel overwhelming because they cover risks, uncertainties, and lifestyle implications honestly. Surgeons assess psychological outlooks because optimism correlates with better recovery trajectories statistically. Patients grappling with unrealistic expectations may struggle more during rehabilitation and satisfaction evaluations. Insurance coverage, rehabilitation program availability, caregiver support systems, and financial planning all enter early discussions. Health professionals aim to build trust by offering balanced, realistic projections without sugarcoating potential difficulties. Establishing honest dialogues from the start lays a stable foundation for the complex months following surgery.
Despite revolutionary advances every surgery still carries inherent risks such as infection blood clots or nerve injury
Even with the finest surgical teams and best hospital environments, complications occasionally surface unpredictably. Postoperative infections, though rare, require immediate attention through antibiotics or additional surgeries if needed. Blood clot prevention protocols include compression devices, early mobilization, and blood-thinning medications. Nerve irritation or damage sometimes causes temporary numbness, tingling, or weakness around surgical sites. Adverse outcomes, while statistically low, remind us that surgery remains a partnership between patient biology and medical expertise. Monitoring recovery symptoms carefully and maintaining scheduled follow-up appointments help detect problems early, preserving best-case scenarios.
Surgeons today use sophisticated navigation systems to improve implant alignment and longevity
Computer-guided systems and robotic arms have transformed joint replacement accuracy, reducing human error significantly. Surgeons map individual anatomical landmarks to guide incision sizes, implant positioning, and ligament balancing. Smaller incisions minimize muscle damage, hasten healing, and lower pain levels during initial recovery. However, even perfect implant placement cannot guarantee perfect movement or sensation immediately after surgery. Rehabilitation remains essential to teaching the body how to move naturally again. Technology enhances possibilities, but human adaptation still writes the final story after the procedure ends.
Conversations before surgery often feel overwhelming because they cover risks uncertainties and lifestyle implications honestly
Hearing about rare but serious complications triggers understandable anxiety among patients preparing for surgery. Discussions about anesthesia risks, mechanical failure rates, or implant rejection possibilities create emotional turbulence. Navigating these conversations with trusted providers builds emotional maturity necessary for post-surgery reality acceptance. Balancing knowledge of risks against the need for surgical intervention sharpens decision-making clarity. Some patients benefit from second opinions, written educational resources, or patient advocacy consultations before proceeding. Informed consent reflects true understanding, not blind optimism or passive compliance.
Even with the finest surgical teams and best hospital environments complications occasionally surface unpredictably
Every biological system behaves slightly differently under surgical stress, complicating universal prediction models. Genetics, underlying chronic conditions, previous surgeries, and even unseen factors like microvascular health influence recovery arcs. Personalized risk assessments create more realistic timelines for expected milestones like walking unaided or returning to work. Discharge planning now includes remote monitoring tools, telemedicine visits, and coordinated outpatient rehabilitation strategies. Despite preparation, a flexible mindset remains essential because detours often arise during complex healing journeys. Success becomes less about avoiding setbacks entirely and more about resilience when facing inevitable hurdles.
Computer-guided systems and robotic arms have transformed joint replacement accuracy reducing human error significantly
Mechanical precision during surgery reduces malalignment risks that historically shortened implant lifespans dramatically. Smart surgical tools adjust in real time based on intraoperative feedback from joint sensors. Tissue-sparing approaches preserve muscles critical for long-term mobility and stability around new joints. These innovations mean faster hospital discharges, shorter initial rehabilitation phases, and lower revision surgery rates. However, overreliance on technology risks ignoring the human factors still governing healing. Trust in tools must remain balanced by respect for biology’s slower, messier processes. Rehabilitation remains an art blending technical skill, patient motivation, and biological patience.
Source: Best Orthopedic Surgeon in Dubai / Best Orthopedic Surgeon in Abu Dhabi